 In a small study comprising (only) 9 patients with disseminated (metastatic) cervical cancer, infusion of activated immune lymphocytes seemingly cured 2 of the terminal subjects, while reducing the tumor burden in one other.
In a small study comprising (only) 9 patients with disseminated (metastatic) cervical cancer, infusion of activated immune lymphocytes seemingly cured 2 of the terminal subjects, while reducing the tumor burden in one other.
One key factor underpinning the theoretical approach to this particular disease cervical cancer is that the overwhelming majority of such tumors are caused by the HPV: human papillomavirus. So the researchers, led by Dr.Christian S. Hinrichs of the National Cancer Institute (NIH, Bethesda MD), activated T-cells from the patients themselves to try to kill off the HPV-related cervical cancer cells. And this technique worked, to an extent.
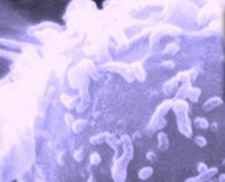
T-cells are the major immune-mediating white blood cells of the body s defenses against foreign invaders such as microbes, and also against the newly-foreign mutations of cancer cells. (In HIV/AIDS, it s the T-cells that are effectively destroyed by the virus, which leads to the numerous infections and cancers that used to kill HIV+ patients before effective antiviral therapies were developed, making AIDS into a chronic disease).
The activated T-cells, harvested from the patients own tumors, were infused in a single procedure, with no significant adverse reactions. Two of the subjects cells demonstrated no reactivity to HPV: they had no response to the T-cell infusion. Among the six patients/subjects whose white blood cells showed reactivity against HPV, half of those (3) did have a response, one partial, two apparently complete: a cure, which has lasted 22 months and 15 months, respectively.
Several experts had commentaries to lend perspective to what amounts to a tiny, yet potentially groundbreaking pilot study. The lead author discussed the study with MedPage Today: It's a proof of principle that immunotherapy -- using what is called adoptive T cell therapy -- can play a role in treating women whose prognosis is otherwise poor, Dr. Hinrichs said at the annual meeting of the American Society of Clinical Oncology. Others noted that, although small, the study did offer a gleam of light in an otherwise dark landscape for women with metastatic cervical cancer. "What has caught our eye is that this is a patient population that has an absolutely dismal prognosis," said Michael Birrer, MD, PhD, of the Massachusetts General Hospital in Boston. (Women with such advanced disease have a median survival of 3.5 months after diagnosis.)
On the other hand, the head of the FDA s division of cancer drugs said this to the NY Times: With anything, all that glitters is not gold, said Dr. Richard Pazdur, who as chief of the cancer division at the F.D.A. has a unique insight into how drugs are performing.


