 By age 50 years, 10% of individuals with normal cognitive function are storing amyloid in their brain, and by age 90 years, 44% of individuals show evidence of amyloid beta (A-β). But, while this plaque deposition is often a harbinger of Alzheimer's disease (AD), patients have AD without amyloid, and amyloid deposition without dementia.
By age 50 years, 10% of individuals with normal cognitive function are storing amyloid in their brain, and by age 90 years, 44% of individuals show evidence of amyloid beta (A-β). But, while this plaque deposition is often a harbinger of Alzheimer's disease (AD), patients have AD without amyloid, and amyloid deposition without dementia.
Moreover, people start to store amyloid in their brain decades before the onset of dementia, with individuals who possess the apolipoprotein E ε4 genotype (APOE-ε4) most vulnerable to amyloid aggregation.
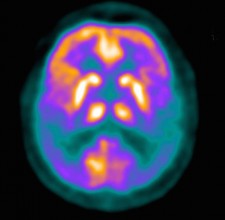
These findings, from two new meta-analyses of the prevalence of amyloid pathology shown on positron-emission tomography (PET) scans of the brain, were published in the May 19 issue of JAMA.
"The finding that amyloid aggregation starts decades before the onset of dementia gives an opportunity for early treatment in the future, but such treatments are not available yet," senior author of the first study, Pieter Jelle Visser, MD, PhD, from Maastricht University in the Netherlands, told Medscape Medical News.
The authors note that the exact interval between the onset of amyloid positivity and onset of AD-type dementia needs to be assessed by long-term follow-up studies because not all persons with amyloid pathology will become demented, and not all individuals with a clinical diagnosis of AD-type dementia have amyloid pathology. "Because of the uncertainty about whether and when an amyloid-positive individual without dementia will develop dementia, amyloid positivity in these individuals should not be equated with impending clinical dementia but rather be seen as a risk state. Our prevalence rates can be used as an inexpensive and noninvasive approach to select persons at risk for amyloid positivity."
The development of Alzheimer s disease pathology may begin as early as 30 years of age, leaving a significant amount of time, approximately 20 to 30 years, between amyloid positivity and the onset of dementia, according to recently published data in JAMA. This study has several implications for understanding the development of AD. The observation that key risk factors for AD-type dementia are also risk factors for amyloid positivity in cognitively normal persons provides further evidence for the hypothesis that amyloid positivity in these individuals reflects early AD, the researchers wrote. Using previously published studies obtained from two medical-scientific databases, researchers evaluated the prevalence of amyloid pathology as measured with biomarkers in patients with normal cognition (2,914), subjective impairment (697), or mild cognitive impairment (3,972).
(Subjective cognitive impairment, SCI, involves concern about waning memory without objective evidence of brain dysfunction; mild cognitive impairment, MCI, is associated with measurable loss of cerebral function that is not so severe as to interfere with most normal daily activities, but it is a significant risk factor for progression to dementia of the AD type).
In all, 55 studies were analyzed, with patients ranging from age 18 years to 100 years. Among patients with normal cognition, the presence of amyloid pathology increased from 10% at age 50 to 44% at age 90. Those with subjective cognitive impairment had an increase from 12% at age 50 to 43% at age 90, and patients with mild cognitive impairment saw an increase from 27% at age 50 to 71% at age 90. Of significance, the researchers noted that AD pathology can develop as early as age 30, meaning that a 20 to 30 year interim between amyloid positivity and dementia may exist, leaving a large portion of time for preventative treatments. Because of the uncertainty about whether and when an amyloidÂ-positive individual without dementia will develop dementia, amyloid positivity in these individuals should not be equated with impending clinical dementia but rather be seen as a risk state, researchers wrote.
In the second meta-analysis, Rik Ossenkoppele, Ph.D., of VU University Medical Center Amsterdam, the Netherlands, and colleagues used individual participant data to estimate the prevalence of amyloid positivity on positron emission tomography (PET) in a wide variety of dementia syndromes. The clinical utility of amyloid PET imaging is potentially limited by a proportion of patients with non-AD dementia and cerebral amyloid-β plaques. To correctly interpret the clinical significance of amyloid PET results, clinicians need to understand the prevalence of amyloid positivity across different types of dementia and how this is associated with demographic, genetic, and cognitive factors. Their findings showed that amyloid deposition is found in other types of dementia e.g., Lewy body dementia, Parkinson s disease but not so commonly as in AD.
ACSH s Dr. Gil Ross had this comment: The current situation, with AD proving to be a major burden on the older population, the millions of caregivers for the approximately 5 million AD patients we now have, and the healthcare structure in general, will soon be dwarfed by a tsunami of aged victims, bereft of identity, memory, all that makes us human. This is the bleak outlook we have, thanks to the increased lifespan bestowed upon society by medical progress and healthier lifestyles. But researchers around the globe are working feverishly to develop remedies to at least slow the march of the disease, and the future portends some approach to predicting populations likely to develop AD decades hence. It is upon those high-risk people that new drug development research will have to be done, for these studies clearly show that we do have a window to impede and eventually prevent the amyloid deposits that may provoke the neuronal destruction leading to dementia.


