After at least 66 documented cases of humans infected with bird flu – which is surely an undercount — the first death was just reported. A 65-year old man with additional medical issues had been exposed to a combination of a backyard flock and wild birds. Ten states reported cases in the grim first week of the New Year.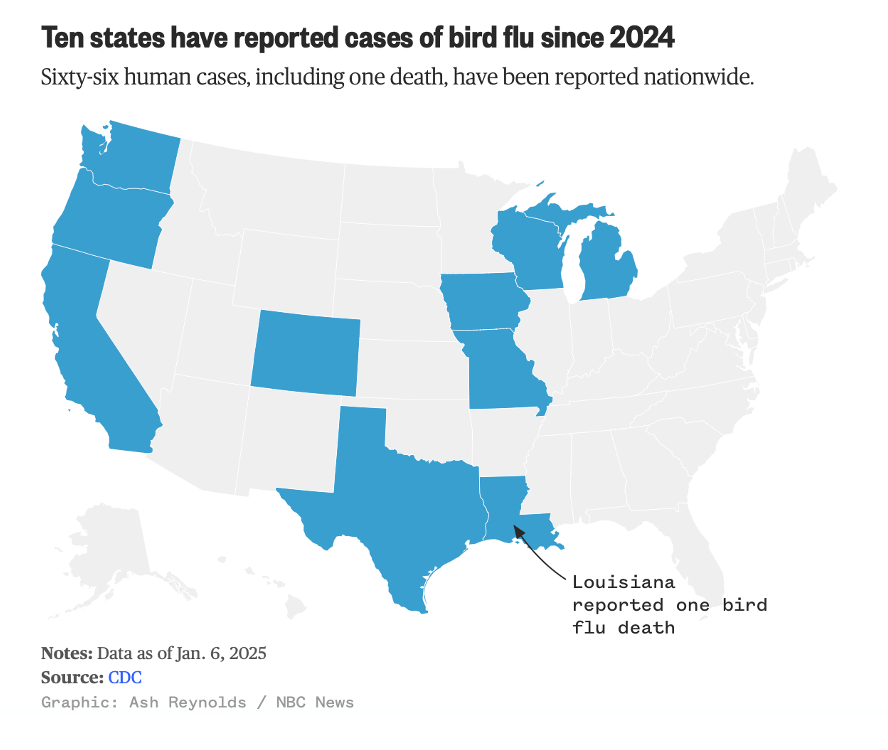
As shown in the CDC's table below, at least two cases in the United States involved patients with no known exposure to animals, heightening concerns that a full-fledged pandemic marked by human-to-human transmission is increasingly possible.
Confirmed human case summary since 2024, by state and exposure source
Exposure Source
| State | Exposure Associated with Commercial Agriculture and Related Operations | Other Animal Exposure† | Exposure Source Unknown‡ | State Total | |
|---|---|---|---|---|---|
| Dairy Herds (Cattle) | Poultry Farms and Culling Operations |
||||
| California | 36 | 0 | 0 | 1 | 37 |
| Colorado | 1 | 9 | 0 | 0 | 10 |
| Iowa | 0 | 1 | 0 | 0 | 1 |
| Louisiana | 0 | 0 | 1 | 0 | 1 |
| Michigan | 2 | 0 | 0 | 0 | 2 |
| Missouri | 0 | 0 | 0 | 1 | 1 |
| Oregon | 0 | 1 | 0 | 0 | 1 |
| Texas | 1 | 0 | 0 | 0 | 1 |
| Washington | 0 | 11 | 0 | 0 | 11 |
| Wisconsin | 0 | 1 | 0 | 0 | 1 |
| Source Total | 40 | 23 | 1 | 2 | 66 |
NOTE: One additional case was previously detected in a poultry worker in Colorado in 2022. Louisiana reported the first H5 bird flu death in the U.S. earlier this month.
†Exposure was related to other animals such as backyard flocks, wild birds, or other mammals
‡Exposure source was not able to be identified
Source: CDC: https://www.cdc.gov/bird-flu/situation-summary/index.html
The H5N1 avian influenza virus, particularly a variant called 2.3.4.4b, has been steadily spreading across the globe since 2021. It has evolved to become capable of infecting a diversity of avian species, marine mammals, cattle, and even, occasionally, humans.
Throughout the U.S., almost a thousand dairy herds have been infected, and more than 130 million poultry have died. (Whenever infection is detected in poultry, the entire flock is culled.) The situation in California is dire. Since the first identification of three infected herds in the state in late August, authorities have found the virus in more than 70% of the state’s 984 dairies, prompting Governor Gavin Newsom to declare an emergency on December 18th. Only last week, outbreaks were detected at three poultry operations in Maryland and Delaware, causing more than 500,000 chickens to be culled and leading to heightened concern among officials in the Washington D.C. region.
Although no sustained human-to-human transmission has been documented, 66 human H5N1 cases have been diagnosed in the U.S. so far this year, and recent genetic studies reveal that the virus might be closer to achieving pandemic potential than previously thought. That would be extremely dangerous, given that infections of humans by previous variants have caused up to 30% mortality.
H5N1 first raised alarms in 1997 when it infected 18 people in Hong Kong, killing six. It has appeared on pandemic watchlists ever since, as researchers uncovered the mutations likely needed to spread efficiently among humans. These mutations involve changes in two viral components: the RNA polymerase, an enzyme that replicates, or copies, the virus’s genome, and hemagglutinin, the protein that enables the virus to latch onto host cells. (During my laboratory days, I was the co-discoverer of the polymerase of the human flu virus.)
Recent studies have amplified scientists’ concerns. A recent report from a research group at the Scripps Research Institute in California found that a single mutation in hemagglutinin — called 226L — was sufficient to allow the virus to bind more effectively to receptors in human airways. Scientists had previously believed two such mutations were necessary, but the discovery of this “shortcut” was alarming because it indicates that adaptation to humans is more advanced than previously predicted.
Canadian warning sign
The case of a Canadian teenager hospitalized with H5N1 last November offers new clues. The virus samples from the patient showed signs of a mutation in hemagglutinin, though not the feared 226L. This suggests that the H5N1 virus may already be “experimenting” with mutations that could eventually lead to human-to-human transmissibility.
The teenager’s virus came from a bird strain that had undergone genetic mixing, or reassortment, of the eight RNA segments that comprise the flu virus’ genome. In this way, the viruses acquired a new neuraminidase protein (the “N” in H5N1), which could make the strain more adaptable.
This is what the CDC reported on December 26 when news arose of the infected Louisiana patient who eventually died:
CDC has sequenced the influenza viruses in specimens collected from the patient in Louisiana who was infected with, and became severely ill from HPAI A(H5N1) virus. The genomic sequences were compared to other HPAI A(H5N1) sequences from dairy cows, wild birds and poultry, as well as previous human cases and were identified as the D1.1 genotype. The analysis identified low frequency mutations in the hemagglutinin gene of a sample sequenced from the patient, which were not found in virus sequences from poultry samples collected on the patient’s property, suggesting the changes emerged in the patient after infection. (Emphasis added.)
The CDC analysis underscores why it is important to “flatten the curve” of infections in humans and animals in order to reduce the number of opportunities for the virus to mutate.
Numbers game
For a flu virus to succeed, its hemagglutinin (H) and neuraminidase (N) proteins must work in harmony. Hemagglutinin binds the virus to host cells, while neuraminidase detaches it, enabling the virus to spread. If the balance is off — too sticky or too loose — the virus fails to proliferate. In the bird strain that infected the Canadian teenager, a new neuraminidase might provide the flexibility needed for hemagglutinin to evolve toward enhanced human infectivity.
One unsettling possibility is that H5N1 already has the mutations needed to spark a pandemic, but its limited spread among humans has kept it in check. The more human exposures to the virus, the greater the chances it will find the right genetic combination.
The occurrence of mutations or advantageous reassortments is all a matter of probability, and the more infections that occur, the more virus replication there is, and the more opportunities for new, worrisome variants to appear that will be winners in Darwinian evolution’s game of survival of the fittest.
(As mentioned above, that is why public health interventions should include “flattening the curve” of infections — to lower the probability of new, more dangerous variants appearing).
Where are we now? As Dr. Jeremy Faust, a Harvard Medical School physician, warns, “our current circumstance is akin to a game of Russian Roulette — and there have never been more bullets in the chamber.”
Surveillance to track genetic changes of the virus is crucial. While the discovery that a lone 226L hemagglutinin mutation could be a potential single-step shortcut to human adaptation is alarming, it doesn’t guarantee a pandemic. Other mutations — such as at certain positions in the polymerase — are likely needed to enable efficient human-to-human spread.
Preparing for the unknown
The case of H5N1 underscores a broader reality about pandemics: They are rare but not impossible. Each mutation brings the virus one step closer to the brink, but predicting whether a virus will cross that threshold remains an uncertain science.
As history has shown, the cost of underestimating a pandemic threat can be devastating. H5N1 may still be contained primarily within animals, but the steady march of new mutations is a reminder that nature can surprise us. Staying one step ahead of the virus could mean the difference between a close call and a global catastrophe.
An earlier version of this article was published by the Genetic Literacy Project.




